Sleep Positions During Pregnancy: What's Safe, What Helps, and How to Actually Rest
Find the best sleeping positions during pregnancy, pillow tips for each trimester, and evidence-based remedies for pregnancy insomnia. Safe, practical advice backed by research.
By Nooko Team

Sleep during pregnancy can feel like a cruel paradox: you’ve never been more tired, yet you’ve never had more trouble sleeping. Between the growing bump, the midnight bathroom trips, the heartburn, and the anxiety about whether you’re lying the “right” way — it’s a lot.
The good news? The science is clearer than the internet makes it seem. This guide covers what the research actually says about sleep positions, how to make yourself comfortable in every trimester, and what to do when sleep simply won’t come.
Why Sleep Position Matters During Pregnancy
As your pregnancy progresses, your sleep position becomes more than a matter of comfort — it can affect blood flow to your baby.
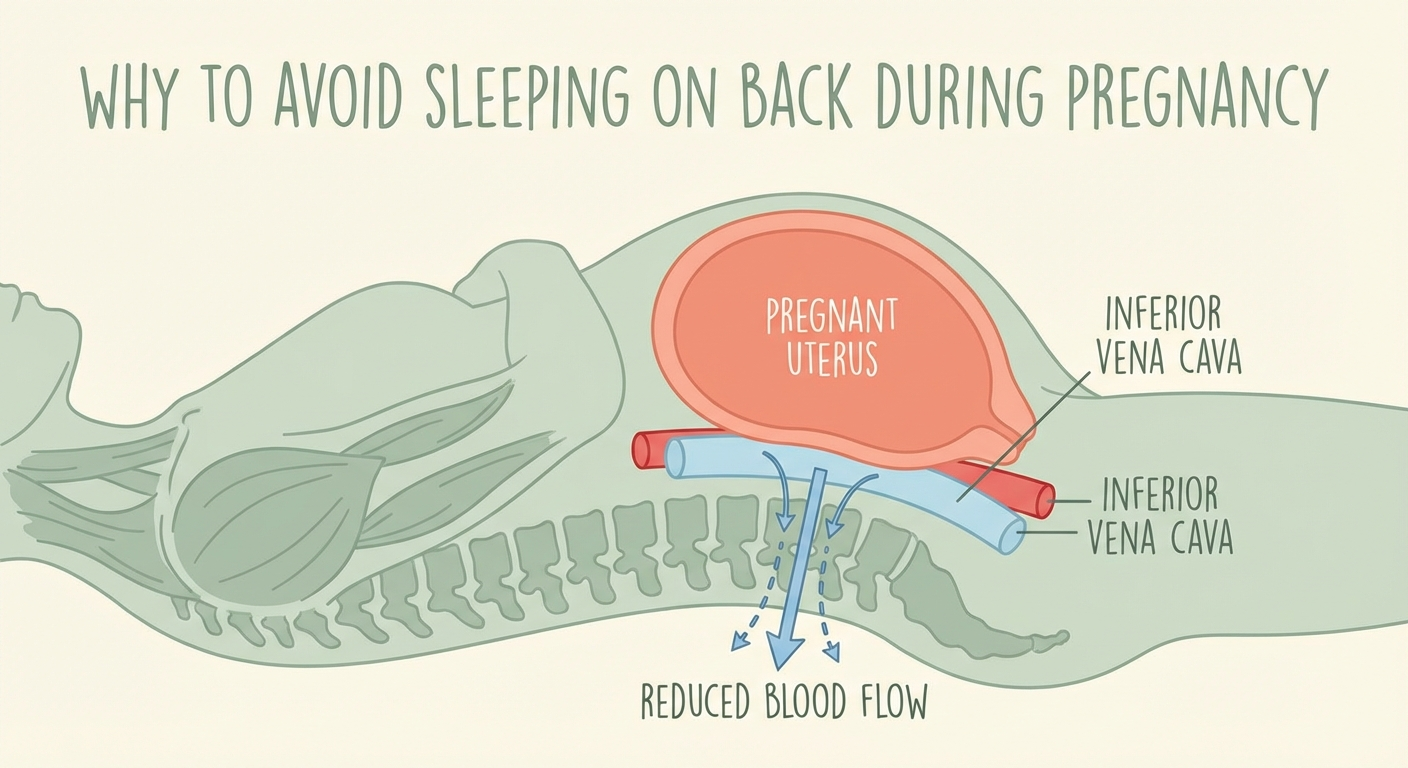
Here’s the anatomy: when you lie flat on your back, the weight of your growing uterus can compress the inferior vena cava, the large vein that returns blood from your lower body to your heart. This compression can reduce cardiac output and blood flow to the placenta (Humphries et al., 2019, The Journal of Physiology).
This doesn’t mean that rolling onto your back for a few minutes will harm your baby. But habitually sleeping on your back in the later stages of pregnancy has been associated with a modestly increased risk of stillbirth in some studies (Stacey et al., 2011, BMJ; Heazell et al., 2018, The Lancet EClinicalMedicine).
The key message: side sleeping is recommended from about 28 weeks onward — but there’s no need to panic if you wake up on your back.
First Trimester (Weeks 1–13): Sleep However You’re Comfortable
During the first trimester, your uterus is still relatively small and tucked within the pelvis. There are no position restrictions at this stage. Sleep on your back, stomach, side — whatever gets you rest.
That said, the first trimester brings its own sleep challenges:
- Extreme fatigue. Rising progesterone levels cause significant drowsiness. You may need 1–2 extra hours of sleep per day.
- Frequent urination. Your kidneys are filtering more blood, and your growing uterus puts pressure on your bladder.
- Nausea. For some, nausea peaks at night or early morning, disrupting sleep.
- Breast tenderness. This can make stomach sleeping uncomfortable earlier than expected.
Tips for the First Trimester
- Nap when you can — even short 20-minute naps help.
- Keep crackers by the bed if nausea wakes you.
- Start reducing caffeine gradually if you haven’t already (NHS recommends no more than 200mg/day during pregnancy).
- Begin a calming bedtime routine — this investment pays off in later trimesters.
Second Trimester (Weeks 14–27): Transitioning to Side Sleeping
As your bump becomes more prominent, stomach sleeping naturally becomes uncomfortable. Many people start shifting to side sleeping during this period.
The Left Side: Is It Really Better?
You’ve probably heard that sleeping on your left side is the gold standard during pregnancy. The reasoning is that it maximises blood flow through the inferior vena cava (which runs slightly to the right of your spine) and optimises perfusion to the placenta, kidneys, and foetus.
The reality is more nuanced. A large study — the MiNESS trial (Heazell et al., 2018) — found that going-to-sleep position on the back after 28 weeks was associated with a higher risk of stillbirth, but it did not find a significant difference between left and right side sleeping.
The current consensus:
- Either side is fine.
- Left side may have a slight theoretical advantage for blood flow.
- The most important thing is to avoid prolonged back sleeping in the third trimester.
- Don’t lose sleep over which side you’re on — the stress of worrying about it is counterproductive.
Pillow Strategies for the Second Trimester
This is when pregnancy pillows start earning their keep:
- Between-the-knees pillow. Placing a pillow between your knees aligns your hips and reduces lower back and pelvic pain. This is the single most recommended modification by physiotherapists.
- Under-the-bump support. A small pillow or folded towel under your belly prevents it from pulling on your back.
- Behind-the-back bolster. If you tend to roll onto your back, a firm pillow behind you provides a gentle reminder to stay on your side.
Third Trimester (Weeks 28–40): Making Side Sleeping Work
By the third trimester, sleep positions matter most — and sleep is hardest to come by. Your bump is large, your bladder is compressed, heartburn peaks, and your body produces relaxin, loosening joints and causing hip discomfort.
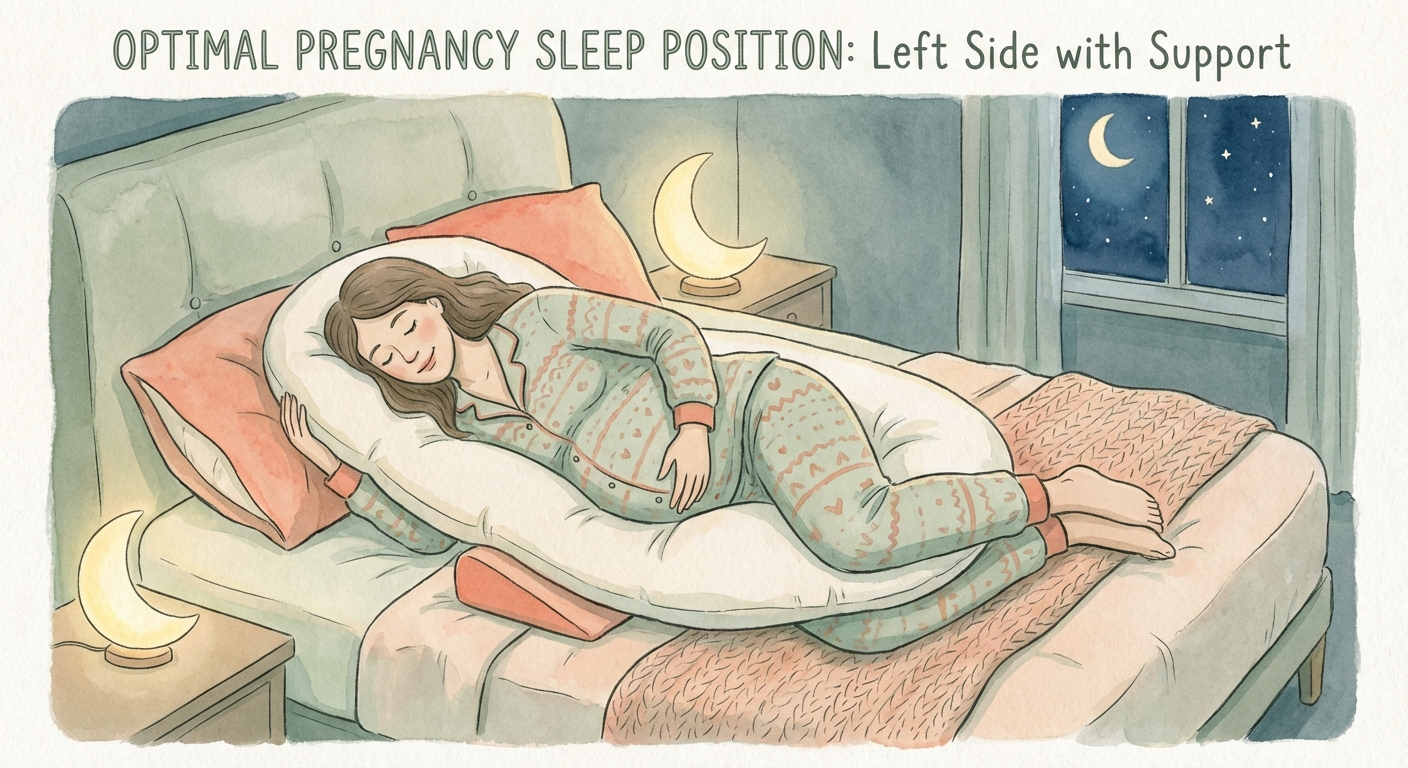
Recommended Position: Side-Lying
The NHS, ACOG, and the Tommy’s charity all recommend going to sleep on your side from 28 weeks onward. This applies to your going-to-sleep position — you can’t control what happens while you’re asleep, and that’s perfectly normal.
If you wake up on your back, simply roll to your side. Research by the Tommy’s charity and the University of Auckland emphasises that the position you fall asleep in is the one you spend the most time in (Gordon et al., 2015, The Journal of Physiology).
The Complete Pillow Setup
Many people find that a full-body pregnancy pillow (C-shaped or U-shaped) transforms their sleep in the third trimester. Here’s what works:
| Pillow Type | Best For | Notes |
|---|---|---|
| C-shaped body pillow | Side sleepers who want head, bump, and knee support in one piece | Curves around your body; supports front only |
| U-shaped body pillow | People who switch sides frequently | Supports both sides so you don’t need to rearrange |
| Wedge pillow | Targeted bump or back support | Compact and portable; great for travel |
| Standard pillow stack | Budget-friendly option | One between knees, one under bump, one behind back |
Additional comfort tips:
- Elevate your upper body slightly if heartburn is an issue. A wedge pillow under your regular pillow can help keep stomach acid where it belongs.
- Keep a pillow between your ankles, not just your knees, if you’re experiencing swelling or varicose veins.
- Try a reclining position if side-lying is truly unbearable. Sleeping in a reclined position (about 45 degrees) in a supportive chair or with pillows can be an acceptable alternative — it avoids full vena cava compression while giving your hips a break.
Pregnancy Insomnia: Why It Happens and What Actually Helps
Insomnia affects up to 78% of pregnant people at some point during pregnancy (Mindell et al., 2015, Sleep Medicine Reviews). It’s not just discomfort — hormonal changes, anxiety, and physiological shifts all contribute.
Common Causes
- Hormonal fluctuations. Progesterone causes daytime drowsiness but can paradoxically disrupt nighttime sleep architecture.
- Physical discomfort. Back pain, hip pain, leg cramps, heartburn, and shortness of breath all interrupt sleep.
- Frequent urination. The pressure on your bladder intensifies as your baby grows, especially in the first and third trimesters.
- Restless legs syndrome (RLS). Affects up to 26% of pregnant people, often worsening in the third trimester (Defined by an irresistible urge to move the legs, usually in the evening; Manconi et al., 2012, Sleep Medicine Reviews).
- Anxiety and racing thoughts. Worries about labour, parenting, finances, and health are entirely normal — but they don’t make for easy sleep.
Evidence-Based Remedies
Sleep Hygiene (The Foundation)
These principles apply to everyone, but they’re especially important during pregnancy when your sleep is already fragile:
- Consistent sleep schedule. Go to bed and wake up at roughly the same time each day, even on weekends.
- Cool, dark, quiet room. Your body temperature is already elevated during pregnancy; a cool room (around 18°C / 65°F) helps. Use blackout curtains and white noise if needed.
- Screen-free wind-down. Stop using phones and laptops at least 30–60 minutes before bed. The blue light suppresses melatonin production.
- Limit fluids in the evening. Stay well-hydrated during the day, but taper off 1–2 hours before bed to reduce nighttime bathroom visits.
- Avoid heavy meals close to bedtime. Eat dinner at least 2–3 hours before sleep. If heartburn is an issue, avoid spicy, acidic, and fatty foods in the evening.
Relaxation Techniques
- Progressive muscle relaxation. Systematically tensing and releasing muscle groups from toes to head. A study in BMC Pregnancy and Childbirth found this improved sleep quality in pregnant participants (Özkan & Rathfisch, 2018).
- Guided breathing. The 4-7-8 technique (inhale 4 seconds, hold 7, exhale 8) activates the parasympathetic nervous system.
- Prenatal meditation apps. Guided meditations designed for pregnancy can help quiet an anxious mind.
- Warm bath before bed. A warm (not hot) bath 1–2 hours before bed can promote sleepiness. Keep water temperature below 38°C (100°F).
Addressing Specific Issues
For heartburn:
- Sleep on your left side (gravity helps keep acid in the stomach).
- Elevate the head of your bed by 10–15 cm.
- Speak to your provider about pregnancy-safe antacids.
For leg cramps:
- Stretch your calves before bed.
- Ensure adequate magnesium and potassium intake (talk to your provider about supplementation).
- Stay hydrated throughout the day.
For restless legs syndrome:
- Have your iron and ferritin levels checked — iron deficiency is a common trigger (Manconi et al., 2012).
- Gentle leg massage or a warm compress before bed may help.
- Avoid caffeine completely if RLS is an issue.
For back and hip pain:
- Use the pillow setup described above.
- Gentle prenatal yoga stretches before bed can ease tension.
- A pregnancy-safe massage can work wonders.
When to Talk to Your Provider
Persistent insomnia isn’t just uncomfortable — chronic sleep deprivation during pregnancy is associated with longer labour, higher rates of caesarean delivery, and increased risk of preterm birth (Chang et al., 2010, Nursing Research). If you’ve tried the strategies above and still can’t sleep:
- Talk to your midwife or doctor. They can rule out underlying conditions (iron deficiency, sleep apnoea, thyroid issues).
- Cognitive Behavioural Therapy for Insomnia (CBT-I) is considered the first-line treatment for chronic insomnia and is safe during pregnancy. It’s more effective than medication in the long term (Manber et al., 2019, Obstetrics & Gynecology).
- Avoid over-the-counter sleep aids without medical advice. Many common sleep medications are not recommended during pregnancy.
What About Stomach Sleeping?
Stomach sleeping in early pregnancy is perfectly safe — your baby is well-protected within the pelvis. As your bump grows, it will naturally become uncomfortable and you’ll shift positions.
Some people use a pregnancy pillow with a cut-out for the belly to maintain a semi-prone position longer. This is fine as long as you’re comfortable and not compressing your bump.
Quick Reference: Sleep Positions by Trimester
| Trimester | Recommended Position | Key Tip |
|---|---|---|
| First (1–13 weeks) | Any comfortable position | Use this time to build good sleep habits |
| Second (14–27 weeks) | Begin transitioning to side sleeping | Introduce a between-the-knees pillow |
| Third (28–40 weeks) | Side sleeping (left or right) | Use a full pillow setup; don’t panic if you wake on your back |
The Bottom Line
Sleep during pregnancy is challenging, but it doesn’t have to be a nightly battle. The evidence is clear: side sleeping from 28 weeks is the safest approach, either side works, and waking up on your back occasionally is not an emergency.
Invest in good pillows, build a consistent bedtime routine, and address specific issues like heartburn or restless legs directly. And if insomnia persists, reach out to your healthcare provider — you deserve rest, and help is available.
Growing a human is hard work. You’ve earned a good night’s sleep.
References
- Chang, J.J., et al. (2010). Sleep deprivation during pregnancy and maternal and fetal outcomes. Nursing Research, 59(1), 60–67.
- Gordon, A., et al. (2015). Sleep position, fetal growth restriction, and late-pregnancy stillbirth. The Journal of Physiology, 125(2), 347–353.
- Heazell, A.E.P., et al. (2018). Association between maternal sleep practices and late stillbirth. The Lancet EClinicalMedicine, 10, 51–58.
- Humphries, A., et al. (2019). The effect of supine positioning on maternal hemodynamics during late pregnancy. The Journal of Physiology, 597(4), 1115–1127.
- Manconi, M., et al. (2012). Restless legs syndrome and pregnancy. Sleep Medicine Reviews, 16(4), 283–295.
- Manber, R., et al. (2019). Cognitive Behavioral Therapy for Insomnia in Pregnancy. Obstetrics & Gynecology, 133(5), 911–919.
- Mindell, J.A., et al. (2015). Sleep patterns and sleep disturbances across pregnancy. Sleep Medicine Reviews, 22, 59–67.
- Özkan, S.A., & Rathfisch, G. (2018). The effect of relaxation exercises on sleep quality in pregnant women. BMC Pregnancy and Childbirth, 18(1), 270.
- Stacey, T., et al. (2011). Association between maternal sleep practices and risk of late stillbirth. BMJ, 342, d3403.
Ready to track your pregnancy?
Join expecting parents using Nooko to track every milestone together.
Join the Nooko Beta →Get Weekly Pregnancy Tips
Expert advice for every stage of your journey
No spam. Privacy policy. Unsubscribe anytime.